What Is Cholesterol?
If you’ve ever wondered about those cholesterol numbers your doctor mentions during checkups, you’re not alone. This guide is designed for anyone who wants to understand cholesterol basics—from people getting their first cholesterol test to those looking to make sense of their results.
Cholesterol affects everyone, but the science behind it doesn’t have to be confusing. We’ll break down the fundamental differences between “good” and “bad” cholesterol and explain how these types impact your heart health. You’ll also learn how your body actually makes cholesterol and what factors—from your diet to your genes—can influence your levels.
By the end, you’ll know how to read your cholesterol test results with confidence and understand what those numbers really mean for your health.
Understanding Cholesterol Fundamentals
What cholesterol is and why your body needs it
Cholesterol is a waxy, fat-like substance that’s absolutely vital for your body’s daily operations. Despite its bad reputation, your body actually produces about 75% of the cholesterol it needs naturally in your liver. The remaining 25% comes from the food you eat.
Think of cholesterol as your body’s construction material and chemical messenger rolled into one. Every single cell in your body contains cholesterol, and without it, you literally couldn’t survive. Your brain alone contains about 25% of your body’s total cholesterol supply, which gives you an idea of just how important this substance really is.
Your body treats cholesterol like a precious resource, carefully regulating its production based on what you consume. When you eat foods high in cholesterol, your liver automatically reduces its own production to maintain balance. This built-in feedback system shows just how crucial cholesterol is for maintaining your health.
How cholesterol differs from other fats in your system
Unlike other fats that your body uses primarily for energy storage, cholesterol serves as a structural component and chemical precursor. While triglycerides can be broken down for fuel when needed, cholesterol maintains its molecular structure and gets recycled throughout your system.
Cholesterol also behaves differently in your bloodstream. Since it doesn’t dissolve in water (or blood), it needs special transport vehicles called lipoproteins to move around your body. This transportation system is unique compared to other fats, which can be processed more directly.
The key difference lies in function: other fats are like fuel for your body’s engine, while cholesterol is more like the engine parts themselves. You can burn fat for energy, but you can’t burn cholesterol – your body repurposes and reuses it instead.
The role cholesterol plays in cell membrane structure
Every cell membrane in your body depends on cholesterol for its structural integrity and flexibility. Cholesterol molecules wedge themselves between other fats in the cell membrane, acting like tiny spacers that keep the membrane at just the right consistency – not too rigid, not too fluid.
This perfect balance allows your cells to:
- Maintain their shape under pressure
- Control what enters and exits the cell
- Respond to chemical signals from other cells
- Adapt to temperature changes
Without adequate cholesterol, your cell membranes would become either too stiff to function properly or too loose to maintain their protective barrier. This is why cholesterol deficiency can be just as problematic as having too much.
Why cholesterol is essential for hormone production
Your body uses cholesterol as the starting material for several critical hormones, including testosterone, estrogen, cortisol, and aldosterone. Without cholesterol, your body simply cannot manufacture these essential chemical messengers.
The process works like this: your body takes cholesterol and modifies it through a series of chemical reactions to create different hormones. Each hormone has a specific job, from regulating your stress response to controlling your reproductive functions.
Cholesterol also helps produce bile acids, which your body needs to digest and absorb fats from food. Your liver converts cholesterol into bile salts, which then help break down dietary fats so your intestines can absorb them properly. This digestive function shows yet another way cholesterol supports your overall health and wellbeing.
Types of Cholesterol and Their Impact on Health
LDL cholesterol and why it’s called “bad” cholesterol
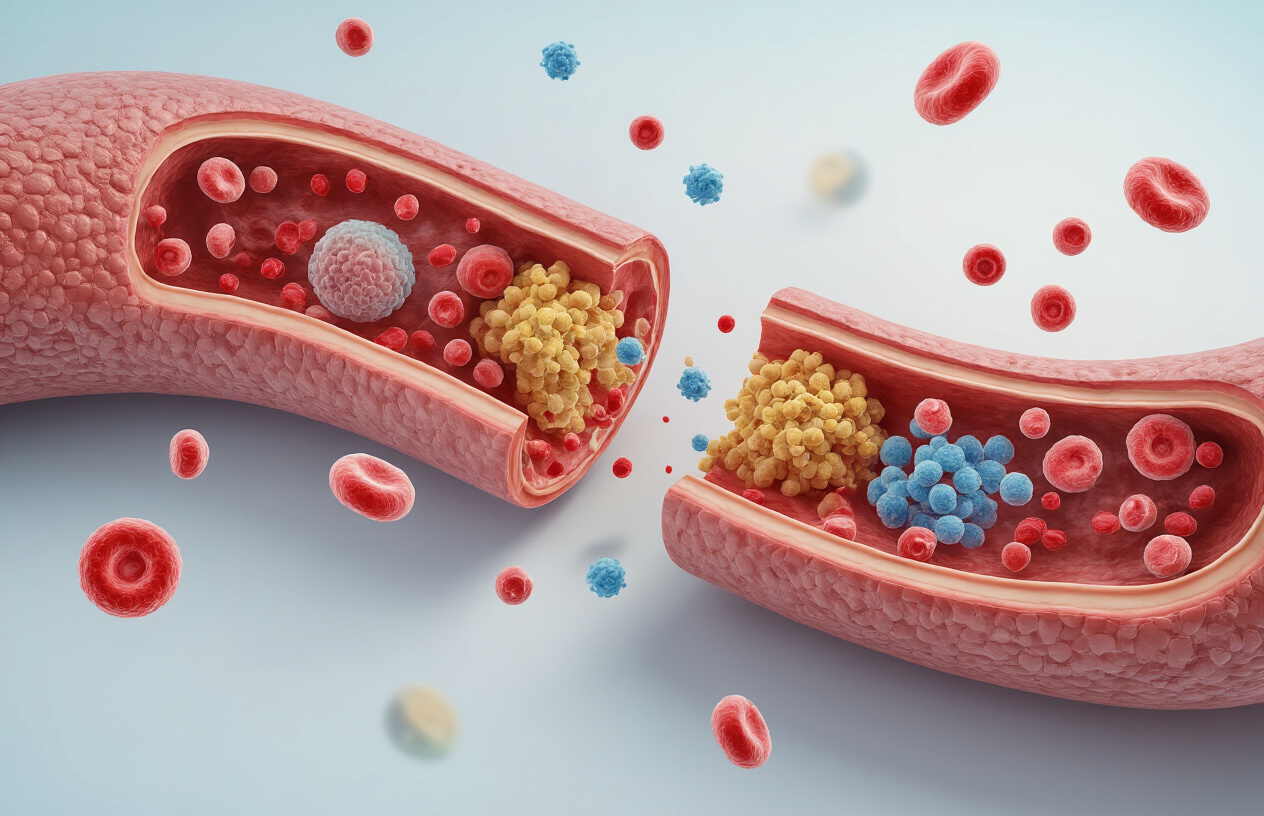
Low-density lipoprotein (LDL) cholesterol earned its notorious reputation as “bad” cholesterol because of what happens when you have too much of it circulating in your bloodstream. Picture LDL particles as delivery trucks carrying cholesterol from your liver to various tissues throughout your body. While this sounds helpful, the problem arises when there’s more cholesterol being delivered than your cells actually need.
When LDL levels become elevated, these particles can infiltrate the walls of your arteries, particularly in areas where blood flow creates turbulence. Once inside the arterial wall, LDL cholesterol undergoes oxidation, triggering an inflammatory response. Your immune system sends white blood cells to deal with this perceived threat, but these cells end up consuming the oxidized LDL and transforming into foam cells. Over time, these foam cells accumulate along with other substances to form atherosclerotic plaques.
These plaques gradually narrow your arteries, reducing blood flow to vital organs like your heart and brain. Even more dangerous is when these plaques become unstable and rupture, potentially causing blood clots that can lead to heart attacks or strokes. The higher your LDL levels, the greater your risk of developing cardiovascular disease. Medical professionals typically recommend keeping LDL cholesterol below 100 mg/dL, with even lower targets for people at high risk.
HDL cholesterol and its protective benefits for your heart
High-density lipoprotein (HDL) cholesterol works like your cardiovascular system’s cleanup crew, which is why doctors call it “good” cholesterol. Unlike LDL, HDL particles travel through your bloodstream collecting excess cholesterol from your tissues and arterial walls, then transporting it back to your liver for disposal or recycling.
The protective mechanism of HDL goes beyond simple cholesterol removal. These particles actively help prevent the oxidation of LDL cholesterol, reducing the inflammatory cascade that leads to plaque formation. HDL also helps maintain the health and flexibility of your blood vessel walls, promoting better circulation and reducing the likelihood of dangerous blood clots.
Research consistently shows an inverse relationship between HDL levels and cardiovascular risk. People with higher HDL cholesterol levels typically have lower rates of heart disease and stroke. Women generally have higher HDL levels than men, which may partially explain why they tend to develop heart disease later in life.
The goal is to maintain HDL levels above 40 mg/dL for men and above 50 mg/dL for women, though higher levels provide even greater protection. Regular exercise, maintaining a healthy weight, avoiding smoking, and consuming moderate amounts of healthy fats can all help boost your HDL levels naturally.
VLDL cholesterol and its connection to triglycerides
Very low-density lipoprotein (VLDL) cholesterol represents the third major type of cholesterol particle, though it’s less commonly discussed than LDL and HDL. VLDL particles are primarily responsible for transporting triglycerides from your liver to various tissues throughout your body. Think of triglycerides as stored energy that your body can use when needed.
The relationship between VLDL and triglycerides is so close that doctors often estimate your VLDL level by dividing your triglyceride level by five. When you eat more calories than your body immediately needs, especially from refined carbohydrates and sugars, your liver converts these excess calories into triglycerides and packages them into VLDL particles for transport and storage.
High VLDL levels contribute to cardiovascular risk in multiple ways. These large, triglyceride-rich particles can directly contribute to atherosclerotic plaque formation. Additionally, elevated VLDL often occurs alongside low HDL and small, dense LDL particles, creating a particularly harmful lipid profile known as atherogenic dyslipidemia.
Normal VLDL levels should remain below 30 mg/dL. When VLDL levels rise above this threshold, they often signal metabolic issues like insulin resistance, diabetes, or metabolic syndrome. Reducing refined carbohydrates, losing excess weight, and increasing physical activity can effectively lower both VLDL cholesterol and triglyceride levels.
How Your Body Produces and Manages Cholesterol

Where cholesterol is made in your body
Your body is actually a cholesterol-making machine, producing about 75-80% of the cholesterol in your bloodstream. The liver takes center stage in this process, cranking out roughly 1,000 milligrams of cholesterol daily. But it’s not the only player in the game.
Your intestines, brain, adrenal glands, and reproductive organs all chip in to manufacture this essential substance. Even your skin cells get in on the action, producing cholesterol to maintain cell membrane integrity. Every single cell in your body has the ability to make cholesterol, though most delegate this job to the liver for efficiency.
The production happens through a complex biochemical pathway that starts with a simple molecule called acetyl-CoA. Your cells convert this into HMG-CoA, then transform it through multiple steps into cholesterol. The enzyme HMG-CoA reductase acts as the key controller in this process – it’s actually the target of statin medications.
How dietary cholesterol affects your blood levels
Here’s where things get interesting: the cholesterol you eat doesn’t directly become the cholesterol in your blood. Your digestive system treats dietary cholesterol differently than your body’s homemade version.
When you eat cholesterol-rich foods like eggs or shellfish, only about 50% gets absorbed through your intestinal wall. The rest gets eliminated as waste. Your body has built-in feedback mechanisms that actually reduce cholesterol production when you consume more through food.
| Cholesterol Source | Daily Amount | Impact on Blood Levels |
|---|---|---|
| Body Production | 1,000mg | Major influence |
| Dietary Intake | 200-400mg | Moderate influence |
| Supplement Form | Varies | Minimal influence |
Most people see only modest increases in blood cholesterol when they increase dietary cholesterol. Some people are “hyper-responders” who experience larger changes, while others show virtually no response to dietary changes.
The liver’s role in cholesterol regulation
Your liver acts like a sophisticated cholesterol control center, constantly monitoring and adjusting production based on your body’s needs. When cholesterol levels drop, the liver ramps up production. When levels rise, it scales back manufacturing.
The liver also manages cholesterol removal through bile acid production. It converts excess cholesterol into bile acids, which help digest fats and eventually get eliminated from your body. This represents one of the few ways your body can actually get rid of cholesterol.
Your liver packages cholesterol into different lipoproteins for transport throughout your body. It creates VLDL particles loaded with triglycerides and cholesterol, which eventually become LDL particles. The liver also produces HDL particles that help transport cholesterol back for processing or disposal.
Why some people produce more cholesterol than others
Genetics play a huge role in determining how much cholesterol your body makes. Some people inherit genes that cause their cells to produce cholesterol like it’s going out of style, while others have more restrained production systems.
Familial hypercholesterolemia affects about 1 in 250 people, causing their bodies to produce excessive amounts of cholesterol regardless of diet or lifestyle. These individuals often have cholesterol levels two to three times higher than average.
Age and hormones also influence production. As you get older, your liver tends to produce more cholesterol. Women typically see increases after menopause when estrogen levels drop. Men generally maintain steadier production throughout life.
Certain medical conditions can throw cholesterol production into overdrive. Diabetes, hypothyroidism, and kidney disease all tend to increase cholesterol manufacturing. Stress hormones like cortisol can also boost production during challenging periods.
Individual variations in enzyme activity mean some people’s cholesterol factories run at different speeds. Your unique genetic blueprint determines how efficiently your HMG-CoA reductase works and how responsive your feedback mechanisms are to changing cholesterol levels.
Factors That Influence Your Cholesterol Levels

Genetic Predisposition and Family History Effects
Your genes play a major role in determining your cholesterol levels, often accounting for up to 60% of the variation between individuals. If your parents or siblings have high cholesterol, you’re more likely to develop it too. This happens because you inherit specific genetic variants that affect how your body produces, processes, and clears cholesterol from your bloodstream.
Some people have familial hypercholesterolemia, a genetic condition that causes extremely high LDL cholesterol levels from birth. Others may inherit genes that make their bodies produce more cholesterol or remove it less efficiently. Even if you eat a healthy diet and exercise regularly, genetic factors can still push your cholesterol levels higher than average.
Family history also reveals shared lifestyle patterns that influence cholesterol. Growing up in a household with certain eating habits or activity levels can create long-lasting patterns that affect your cholesterol throughout life.
Diet Choices That Raise or Lower Cholesterol
What you eat directly impacts your cholesterol levels, though the relationship is more complex than many people realize. Saturated fats found in red meat, full-fat dairy products, and tropical oils can raise LDL cholesterol. Trans fats, often hiding in processed foods and baked goods, are even worse for your cholesterol profile.
Foods that help lower cholesterol include:
- Soluble fiber from oats, beans, and apples
- Nuts like almonds and walnuts
- Fatty fish rich in omega-3 fatty acids
- Plant sterols and stanols found in fortified foods
- Olive oil and other healthy fats
Dietary cholesterol from eggs and shellfish has less impact on blood cholesterol than previously thought. Your liver adjusts its own cholesterol production based on what you consume, so eating cholesterol doesn’t automatically raise blood levels for most people.
Physical Activity’s Impact on Cholesterol Balance
Exercise creates powerful changes in your cholesterol profile that go beyond simple weight loss. Regular physical activity raises HDL cholesterol while lowering LDL cholesterol and triglycerides. Even moderate exercise like brisk walking for 30 minutes most days can improve your numbers.
Different types of exercise offer unique benefits:
- Aerobic activities like running and cycling boost HDL production
- Resistance training helps reduce LDL cholesterol
- High-intensity interval training can improve overall cholesterol ratios
Exercise also increases the size of LDL particles, making them less likely to stick to artery walls. This particle size change happens regardless of weight loss, showing that exercise benefits cholesterol through multiple biological pathways.
Age and Gender Differences in Cholesterol Management
Cholesterol levels naturally change as you age, following different patterns for men and women. Men typically see cholesterol levels peak in their 40s and 50s, while women often experience significant increases after menopause when estrogen levels drop.
Before menopause, women generally have higher HDL cholesterol and lower LDL cholesterol than men of the same age. Estrogen provides protective effects that help maintain healthy cholesterol ratios. After menopause, these advantages disappear, and women’s cholesterol profiles often worsen rapidly.
Age-related changes include:
- Slower metabolism affecting cholesterol processing
- Decreased physical activity impacting HDL levels
- Hormonal changes altering cholesterol production
- Increased insulin resistance affecting triglycerides
Medical Conditions That Affect Cholesterol Levels
Several health conditions can significantly alter your cholesterol levels, sometimes making lifestyle changes less effective. Diabetes often comes with high triglycerides and low HDL cholesterol, creating a challenging lipid profile that requires careful medical management.
Thyroid disorders have dramatic effects on cholesterol. An underactive thyroid can cause cholesterol levels to skyrocket, while an overactive thyroid might lower them too much. Kidney disease, liver problems, and certain autoimmune conditions also disrupt normal cholesterol metabolism.
Common medications can influence cholesterol levels:
- Beta-blockers may lower HDL cholesterol
- Diuretics can raise LDL cholesterol and triglycerides
- Corticosteroids often increase total cholesterol
- Some antidepressants affect lipid metabolism
Polycystic ovary syndrome (PCOS) in women frequently causes insulin resistance, leading to higher triglycerides and lower HDL cholesterol. Sleep apnea, chronic kidney disease, and metabolic syndrome all create inflammatory conditions that worsen cholesterol profiles and increase cardiovascular risk.
Reading and Understanding Cholesterol Test Results
What the numbers mean in your lipid panel
When you get your cholesterol test results back, you’ll see several numbers that might look like a foreign language at first. Your lipid panel typically includes four key measurements that paint a complete picture of your cardiovascular health.
Total cholesterol represents the sum of all cholesterol types in your blood, measured in milligrams per deciliter (mg/dL). While this number gives you a baseline, it doesn’t tell the whole story about your heart health risk.
LDL cholesterol, often called “bad” cholesterol, shows how much low-density lipoprotein is circulating in your bloodstream. This type tends to build up in your artery walls, creating blockages over time. Lower numbers here are definitely better.
HDL cholesterol is your “good” cholesterol that actually helps remove other forms of cholesterol from your arteries and transport them back to your liver for disposal. Higher HDL numbers work in your favor.
Triglycerides measure the fats in your blood that come primarily from the food you eat. Your body converts excess calories, sugar, and alcohol into triglycerides and stores them in fat cells for later energy use.
Some labs also include additional measurements like non-HDL cholesterol (total minus HDL) or cholesterol ratios, which help doctors get an even clearer picture of your cardiovascular risk profile.
Optimal cholesterol ranges for different age groups
Cholesterol targets aren’t one-size-fits-all numbers. Your age, gender, and existing health conditions all play important roles in determining what levels are right for you.
| Age Group | Total Cholesterol | LDL | HDL | Triglycerides |
|---|---|---|---|---|
| Children & Teens | Less than 170 mg/dL | Less than 100 mg/dL | More than 45 mg/dL | Less than 75 mg/dL |
| Adults 20+ | Less than 200 mg/dL | Less than 100 mg/dL | 40+ mg/dL (men), 50+ mg/dL (women) | Less than 150 mg/dL |
For adults over 40, doctors often focus more on your 10-year cardiovascular disease risk rather than just looking at isolated numbers. Someone with diabetes, high blood pressure, or a family history of heart disease might need more aggressive LDL targets, sometimes below 70 mg/dL.
Women after menopause often see their cholesterol levels change due to hormonal shifts. HDL levels may drop while LDL and total cholesterol tend to rise, making regular monitoring even more important.
Older adults (65+) might have slightly different target ranges, especially if they have other health conditions. The focus often shifts to preventing immediate cardiovascular events rather than long-term prevention.
When to be concerned about your cholesterol levels
Red flags in your cholesterol results aren’t always obvious, and sometimes “borderline” numbers deserve attention too. Your total cholesterol hitting 240 mg/dL or higher definitely warrants concern, but even levels between 200-239 mg/dL put you in the borderline-high category.
LDL levels above 160 mg/dL signal that you’re at increased risk for heart disease, especially if you have other risk factors. However, people with existing heart disease or diabetes should worry when their LDL climbs above 100 mg/dL, and some may need to keep it under 70 mg/dL.
Low HDL levels are just as concerning as high LDL. Men with HDL below 40 mg/dL and women below 50 mg/dL face higher cardiovascular risks. Think of HDL as your cleanup crew – when those numbers drop, less cholesterol gets removed from your arteries.
Triglycerides over 150 mg/dL start raising eyebrows, and levels above 500 mg/dL can actually trigger dangerous inflammation in your pancreas. High triglycerides often travel with other problems like obesity, diabetes, or metabolic syndrome.
Pay attention to trends in your numbers over time. Even if your cholesterol sits in the “normal” range, steadily climbing levels over several years might indicate developing problems. Your doctor will also consider your complete health picture – family history, blood pressure, smoking status, and other conditions – when deciding if your cholesterol levels should concern you.

Cholesterol plays a much bigger role in your health than most people realize. Your body actually needs this waxy substance to build healthy cells and produce important hormones, but the balance between good HDL and bad LDL cholesterol makes all the difference. When you understand how your liver produces cholesterol and what factors like diet, exercise, genetics, and lifestyle choices affect your levels, you can take control of your heart health.
Getting regular cholesterol tests and knowing how to read those numbers gives you the power to make informed decisions about your wellbeing. Talk to your doctor about scheduling a lipid panel if you haven’t had one recently, and don’t wait until there’s a problem. Small changes in your daily habits today can lead to healthier cholesterol levels and a stronger cardiovascular system for years to come.









