Diabetes mellitus affects over 400 million people worldwide and can seriously impact your daily life if left unmanaged. This guide is for anyone who wants to understand diabetes better—whether you’re newly diagnosed, have a family history of the condition, or simply want to learn about this common health issue.
We’ll break down the main causes behind diabetes development, from genetic factors to lifestyle choices that increase your risk. You’ll also learn how to spot the early warning signs and symptoms that often go unnoticed, plus discover the key differences between Type 1, Type 2, and other forms of diabetes. Finally, we’ll explore practical management strategies that can help you or your loved ones live well with this condition.
Understanding Diabetes Mellitus and Its Impact on Your Health

What diabetes mellitus means for your body’s glucose processing
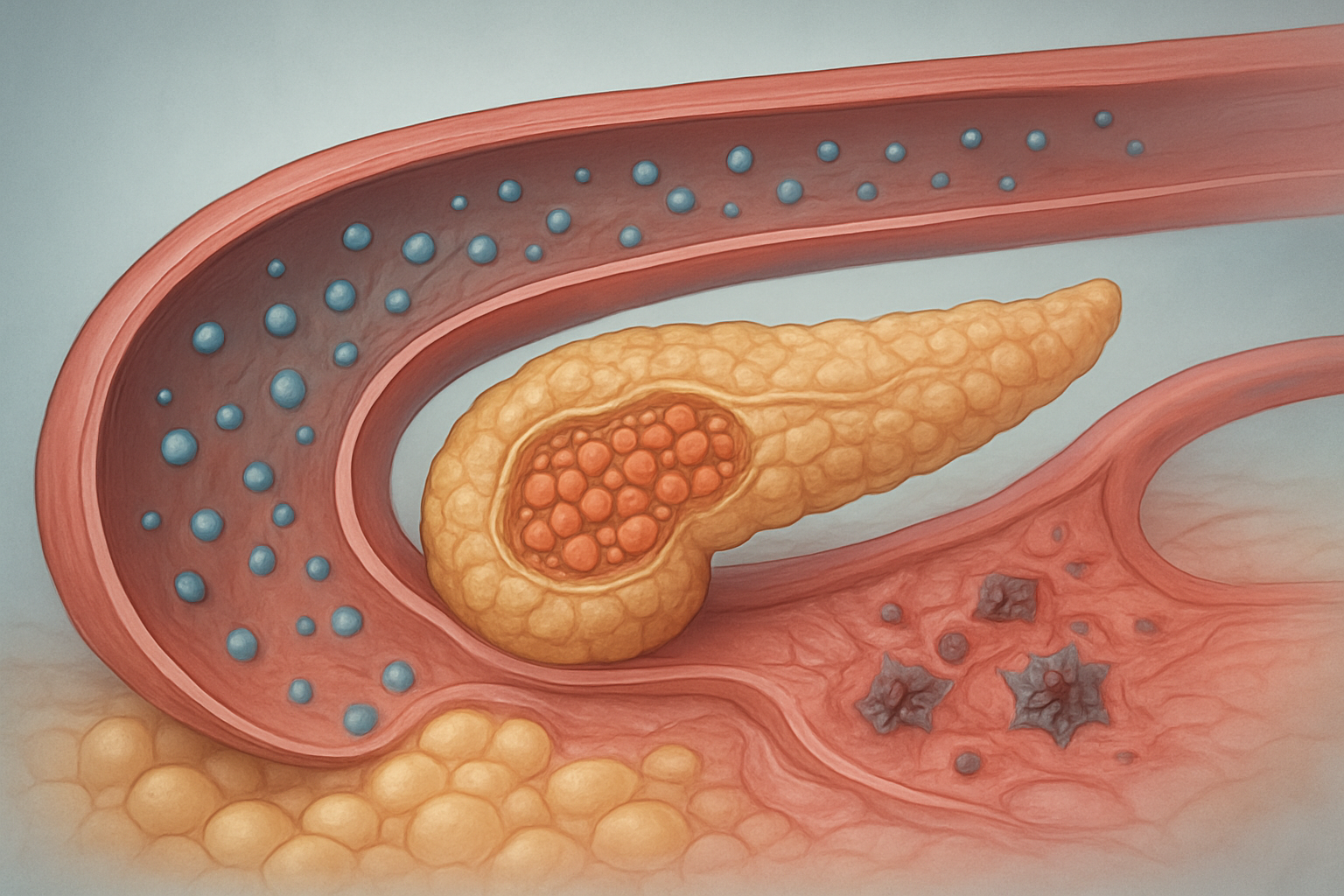
Diabetes mellitus disrupts your body’s natural ability to manage blood sugar, creating a cascade of health challenges that affect nearly every system in your body. When you eat, your digestive system breaks down carbohydrates into glucose, which enters your bloodstream. Normally, your pancreas responds by releasing insulin, a hormone that acts like a key, unlocking your cells so glucose can enter and provide energy.
In diabetes, this process breaks down in one of two main ways. Either your pancreas stops producing enough insulin, or your cells become resistant to insulin’s effects, leaving glucose trapped in your bloodstream. This creates dangerously high blood sugar levels that, over time, damage your blood vessels, nerves, kidneys, eyes, and heart.
Think of insulin as a delivery truck that carries glucose to hungry cells throughout your body. Without enough trucks or when the delivery doors are jammed shut, glucose piles up in your bloodstream like packages with nowhere to go. Your cells starve for energy while your blood becomes thick and syrupy with excess sugar, creating the perfect environment for serious complications.
How diabetes affects millions worldwide and why it matters to you
Over 537 million adults worldwide live with diabetes, and this number continues climbing at an alarming rate. Every 5 seconds, someone develops diabetes, making it one of the fastest-growing health conditions globally. The financial burden exceeds $966 billion annually in healthcare costs, disability, and lost productivity.
These statistics aren’t just numbers – they represent your neighbors, coworkers, family members, and possibly your future self. Diabetes doesn’t discriminate based on age, income, or background, though certain factors increase your risk. The condition has become so common that most people know someone affected by it.
What makes these numbers particularly concerning is that many cases remain undiagnosed. Nearly 1 in 3 people with diabetes don’t know they have it, walking around with dangerously high blood sugar levels that silently damage their bodies. This hidden epidemic means the actual impact is likely much larger than current statistics suggest.
The personal cost extends beyond medical bills. Diabetes can affect your career, relationships, and daily activities. Simple pleasures like family meals become medical calculations, and spontaneous activities require careful planning around blood sugar management.
The difference between diabetes and other blood sugar conditions
Blood sugar disorders exist on a spectrum, with diabetes representing the most serious end. Prediabetes sits in the middle ground, where your blood sugar levels are higher than normal but not yet high enough for a diabetes diagnosis. Think of prediabetes as your body’s warning system – blood sugar levels between 100-125 mg/dL when fasting signal that your glucose processing system is struggling but hasn’t completely failed yet.
Hypoglycemia, or low blood sugar, creates the opposite problem. Your blood glucose drops below normal levels (typically under 70 mg/dL), causing shakiness, confusion, and potentially dangerous symptoms. While people with diabetes often experience hypoglycemia as a side effect of treatment, it can also occur in people without diabetes due to various medical conditions or medications.
| Condition | Fasting Blood Glucose | Key Characteristics |
|---|---|---|
| Normal | 70-99 mg/dL | Healthy glucose processing |
| Prediabetes | 100-125 mg/dL | Warning stage, reversible |
| Diabetes | 126+ mg/dL | Requires lifelong management |
| Hypoglycemia | Below 70 mg/dL | Immediate treatment needed |
Gestational diabetes develops during pregnancy and usually disappears after delivery, though it increases the risk of developing type 2 diabetes later. Reactive hypoglycemia causes blood sugar to drop several hours after eating, creating symptoms similar to diabetes-related low blood sugar but with different underlying causes.
Why early detection can transform your health outcomes
Catching diabetes early dramatically changes your health trajectory and quality of life. When diagnosed in the prediabetes stage, you can often prevent or delay the progression to full diabetes through lifestyle changes. Studies show that losing just 7% of your body weight and exercising 150 minutes per week can reduce your diabetes risk by 58%.
Early detection also prevents the devastating complications that make diabetes so dangerous. High blood sugar levels damage blood vessels and nerves gradually over years, often without obvious symptoms. By the time people notice problems like vision changes, numbness in their feet, or frequent infections, significant damage has already occurred.
Regular screening becomes your best defense, especially if you have risk factors like family history, obesity, or a sedentary lifestyle. Simple blood tests can detect problems years before symptoms appear, giving you time to take action. The hemoglobin A1C test reveals your average blood sugar levels over the past 2-3 months, providing a clear picture of your glucose processing ability.
People diagnosed early have more treatment options and better outcomes. They can often manage their condition with lifestyle changes alone, avoiding the need for multiple medications or insulin injections. Early intervention also reduces the risk of heart disease, stroke, kidney failure, and other serious complications by up to 40%.
Your healthcare provider can help determine your screening schedule based on your individual risk factors, but most adults should have their blood sugar checked at least every three years starting at age 35.
Root Causes Behind Diabetes Development
Genetic factors that increase your diabetes risk
Your genes play a major role in determining whether you’ll develop diabetes. If your parents or siblings have diabetes, your chances increase significantly. Type 1 diabetes has strong genetic links – having a parent with this condition gives you about a 1 in 17 chance of developing it yourself. Type 2 diabetes shows even stronger family patterns, with your risk jumping to 40% if both parents have the condition.
Specific genes control how your body makes and uses insulin. Some people inherit variations that make their pancreas produce less insulin or cause their cells to resist insulin’s effects. Researchers have identified over 120 genetic variants linked to Type 2 diabetes risk. While you can’t change your genes, knowing your family history helps you take preventive steps early.
Lifestyle choices that trigger diabetes onset
Your daily habits directly impact your diabetes risk. Poor eating patterns top the list – consuming too much processed food, sugary drinks, and refined carbs overwhelm your body’s ability to manage blood sugar. Regular consumption of fast food doubles your diabetes risk compared to eating it less than twice weekly.
Physical inactivity creates a perfect storm for diabetes development. Sitting for long periods and skipping exercise make your muscles less sensitive to insulin. Even moderate activity like brisk walking for 30 minutes daily can reduce your risk by 30%. Sleep also matters – getting less than six hours nightly increases diabetes risk by 28%.
Chronic stress triggers hormone release that raises blood sugar levels over time. Poor stress management, whether from work pressure or personal challenges, keeps these harmful hormones elevated.
Environmental triggers you can identify and avoid
Your surroundings influence diabetes development more than you might realize. Air pollution exposure increases diabetes risk by 20-40%. Living near busy roads or industrial areas means breathing particles that cause inflammation and insulin resistance.
Chemical exposures also matter. Pesticides, plastics containing BPA, and certain household cleaners disrupt your endocrine system. These chemicals interfere with normal hormone function, including insulin production and effectiveness.
Your neighborhood environment shapes your health choices too. Limited access to fresh groceries, unsafe walking areas, and lack of recreational facilities make healthy living harder. Food deserts – areas without affordable, nutritious food options – show higher diabetes rates.
| Environmental Factor | Impact on Diabetes Risk |
|---|---|
| Air pollution | 20-40% increased risk |
| Chemical exposure | Hormone disruption |
| Food deserts | Limited healthy options |
| Unsafe neighborhoods | Reduced physical activity |
How age and ethnicity influence your diabetes susceptibility
Age brings natural changes that increase diabetes risk. After 45, your risk rises sharply every decade. Your pancreas produces less insulin as you age, and your muscle mass decreases, reducing your body’s ability to use glucose effectively. Hormonal changes during menopause also affect blood sugar control in women.
Ethnicity creates distinct risk patterns. African Americans face twice the diabetes risk of white Americans, developing the condition earlier and experiencing more complications. Hispanic Americans, especially those of Mexican descent, show similar elevated risks. Asian Americans develop diabetes at lower body weights than other groups, suggesting different genetic sensitivities.
Native Americans have the highest diabetes rates globally – some tribes see rates exceeding 50% of adults. These disparities stem from genetic factors, historical trauma affecting stress levels, and limited access to healthcare and healthy foods on reservations.
Medical conditions that lead to secondary diabetes
Several health conditions can trigger diabetes development. Polycystic ovary syndrome (PCOS) affects 1 in 10 women and triples diabetes risk through insulin resistance. The hormonal imbalances in PCOS make blood sugar control difficult even before diabetes develops.
Cushing’s syndrome, where your body produces too much cortisol, directly causes high blood sugar. This stress hormone tells your liver to release more glucose while making your cells resistant to insulin.
Pancreatic diseases like pancreatitis or pancreatic cancer damage insulin-producing cells. Even after recovery, your pancreas may never produce normal insulin amounts. Certain medications also increase diabetes risk – steroids, some blood pressure medications, and antipsychotic drugs can all affect blood sugar control.
Gestational diabetes during pregnancy signals future Type 2 diabetes risk. Women who develop diabetes while pregnant have a 50% chance of developing permanent diabetes within 10 years. The pregnancy hormones that cause gestational diabetes reveal underlying insulin resistance that often persists after delivery.
Recognizing Early Warning Signs and Symptoms

Classic symptoms that signal high blood sugar levels
The most recognizable warning signs of diabetes revolve around your body’s struggle to properly use glucose for energy. Excessive thirst and frequent urination work as a tag team – when blood sugar levels climb too high, your kidneys work overtime to filter out the excess glucose, pulling water from your tissues and leaving you dehydrated. This creates an endless cycle where you drink more water, which leads to more trips to the bathroom.
Unexplained weight loss often catches people off guard, especially when they’re eating normally or even more than usual. Your body starts breaking down muscle and fat for energy when it can’t access glucose properly. Extreme fatigue becomes a constant companion as your cells literally starve for energy despite having plenty of glucose floating around in your bloodstream.
Increased hunger, known medically as polyphagia, happens because your cells send distress signals demanding more fuel. Blurred vision occurs when high blood sugar levels cause the lens in your eye to swell, changing its shape and affecting your ability to focus clearly.
Subtle signs you might overlook but shouldn’t ignore
Beyond the obvious symptoms, diabetes often announces itself through quieter signals that many people dismiss as stress or aging. Slow-healing cuts and wounds happen because high blood sugar damages blood vessels and impairs your immune system’s ability to fight infection and promote healing.
Recurring infections, particularly urinary tract infections, yeast infections, and skin infections, become more common as elevated glucose levels create an ideal environment for bacteria and fungi to thrive. Your body’s natural defense mechanisms weaken under the constant strain of managing excess sugar.
Tingling or numbness in your hands and feet signals potential nerve damage from prolonged high blood sugar levels. This diabetic neuropathy often starts as a mild sensation that people attribute to poor circulation or sleeping in an awkward position.
Dark, velvety patches of skin called acanthosis nigricans commonly appear around the neck, armpits, or groin area. These patches often indicate insulin resistance and can appear years before diabetes develops. Dry, itchy skin results from dehydration and poor circulation, while gum disease and dental problems increase due to reduced saliva production and higher glucose levels in your saliva.
How symptoms differ between diabetes types
Type 1 diabetes typically announces itself with dramatic, rapid-onset symptoms that develop over weeks or months. The classic triad of excessive thirst, frequent urination, and weight loss appears quickly and intensely. People with Type 1 often experience diabetic ketoacidosis, a life-threatening condition where the body produces dangerous levels of ketones, causing symptoms like vomiting, abdominal pain, and fruity-smelling breath.
Type 2 diabetes plays a more subtle game, with symptoms developing gradually over years. Many people live with elevated blood sugar levels for extended periods before noticing obvious signs. The weight loss seen in Type 1 is less common in Type 2, where weight gain or difficulty losing weight is more typical. Fatigue in Type 2 diabetes tends to be less severe and more easily attributed to other factors like stress or lack of sleep.
Gestational diabetes often produces no noticeable symptoms, which is why routine screening during pregnancy is so important. When symptoms do appear, they mirror Type 2 diabetes but are usually milder.
| Diabetes Type | Onset Speed | Primary Symptoms | Unique Features |
|---|---|---|---|
| Type 1 | Rapid (weeks to months) | Severe thirst, frequent urination, weight loss | Ketoacidosis, fruity breath |
| Type 2 | Gradual (months to years) | Mild fatigue, slow healing, infections | Often asymptomatic initially |
| Gestational | Variable | Usually none to mild | Detected through screening |
When to seek immediate medical attention
Certain combinations of symptoms demand urgent medical care and shouldn’t wait for a regular doctor’s appointment. Diabetic ketoacidosis presents with vomiting, severe abdominal pain, rapid breathing, fruity-smelling breath, and confusion. This medical emergency requires immediate hospitalization and can be fatal without prompt treatment.
Hyperosmolar hyperglycemic state, more common in Type 2 diabetes, causes extreme dehydration, altered mental state, and blood sugar levels exceeding 600 mg/dL. Signs include severe confusion, weakness, and sometimes seizures or loss of consciousness.
Any combination of classic diabetes symptoms – excessive thirst, frequent urination, unexplained weight loss, and extreme fatigue – warrants prompt medical evaluation, especially if they develop rapidly or interfere with daily activities. Blood sugar readings above 250 mg/dL on a home glucose meter, persistent vomiting that prevents keeping fluids down, or signs of severe dehydration like dizziness, rapid heartbeat, or decreased urination all require immediate medical attention.
Don’t ignore recurring infections that don’t respond to treatment, wounds that won’t heal after several weeks, or sudden changes in vision. These symptoms might indicate diabetes complications that need professional management to prevent permanent damage.
Essential Types of Diabetes You Need to Know

Type 1 Diabetes Characteristics and Who It Affects Most
Type 1 diabetes strikes when the body’s immune system turns against itself, destroying the insulin-producing beta cells in the pancreas. This autoimmune attack leaves people unable to produce insulin naturally, making blood sugar regulation impossible without external intervention.
The condition typically shows up during childhood or teenage years, earning it the nickname “juvenile diabetes.” However, adults can develop Type 1 diabetes too, sometimes called latent autoimmune diabetes in adults (LADA). About 5-10% of all diabetes cases fall into this category.
Unlike other forms of diabetes, Type 1 doesn’t discriminate based on weight or lifestyle choices. Even the healthiest, most active kids can develop this condition. Genetics play a significant role, with certain gene combinations increasing risk, but having family members with Type 1 diabetes doesn’t guarantee you’ll get it.
People with Type 1 diabetes need daily insulin injections or an insulin pump to survive. Their bodies simply can’t make this crucial hormone anymore. The onset often happens quickly, with symptoms appearing over weeks rather than years.
Type 2 Diabetes Development and Risk Factors
Type 2 diabetes develops differently, usually creeping up gradually over months or years. The body still produces insulin, but cells become resistant to its effects, or the pancreas doesn’t make enough to keep blood sugar levels normal.
Age becomes a major factor, with risk increasing significantly after 45. However, Type 2 diabetes now affects younger people more frequently due to rising obesity rates and sedentary lifestyles. Weight plays a crucial role – carrying excess pounds, especially around the midsection, dramatically increases your chances.
Family history matters here too. Having parents or siblings with Type 2 diabetes roughly doubles your risk. Certain ethnic groups face higher odds, including African Americans, Hispanic Americans, Native Americans, and Asian Americans.
Lifestyle factors create a perfect storm for Type 2 development:
- Physical inactivity – Regular exercise helps muscles use glucose effectively
- Poor diet – High-calorie, processed foods contribute to weight gain and insulin resistance
- High blood pressure – Often accompanies diabetes and increases complications
- Abnormal cholesterol levels – Low HDL or high triglycerides signal metabolic problems
Previous gestational diabetes or delivering a baby weighing over 9 pounds also raises risk levels significantly.
Gestational Diabetes During Pregnancy and Its Implications
Pregnancy brings many changes, including how the body processes sugar. Gestational diabetes develops when hormones from the placenta interfere with insulin’s effectiveness, typically appearing between weeks 24-28 of pregnancy.
This condition affects about 2-10% of pregnancies annually in the United States. Risk factors include being over 25, having a family history of diabetes, previous gestational diabetes, or belonging to certain ethnic groups with higher diabetes rates.
The implications extend beyond pregnancy itself. For mothers, gestational diabetes increases the likelihood of developing Type 2 diabetes later in life – studies show up to 50% will develop it within 5-10 years after delivery. High blood pressure during pregnancy also becomes more common.
Babies face their own risks when mothers have gestational diabetes:
| Risk | Description |
|---|---|
| Macrosomia | Excessive birth weight (over 9 lbs) |
| Birth complications | Shoulder dystocia, cesarean delivery |
| Hypoglycemia | Low blood sugar after birth |
| Respiratory distress | Breathing problems at birth |
| Future diabetes risk | Higher chance of obesity and Type 2 diabetes |
The good news? Proper management during pregnancy usually leads to healthy outcomes for both mother and baby. Many women control gestational diabetes through diet and exercise alone, though some need insulin injections. Blood sugar levels typically return to normal after delivery, but regular screening remains important for early detection of Type 2 diabetes.
Taking Control Through Effective Management Strategies

Blood sugar monitoring techniques that work best
Modern glucose monitoring gives you real-time insights into how your body responds to food, activity, and stress. Traditional fingerstick meters remain the gold standard for most people with diabetes. Check your levels before meals, two hours after eating, and at bedtime to establish patterns. Clean hands matter more than alcohol swabs – soap and warm water provide the most accurate readings.
Continuous glucose monitors (CGMs) have revolutionized diabetes care by providing 24/7 data without constant finger pricks. These devices show trends and alert you to dangerous highs or lows before they become emergencies. While more expensive upfront, CGMs often reduce long-term complications and improve quality of life.
Keep detailed logs that include blood sugar readings, meal times, exercise, medications, and how you feel. Many smartphone apps sync with glucose meters to track this information automatically. Look for patterns – maybe your morning coffee spikes your glucose, or stress at work consistently raises your levels.
The key is finding a monitoring routine you’ll actually stick with. Some people thrive on checking multiple times daily, while others prefer the freedom of a CGM. Work with your healthcare team to determine the right frequency and timing for your specific needs and diabetes type.
Dietary changes that stabilize your glucose levels
Carbohydrate counting forms the foundation of effective diabetes nutrition. Every 15 grams of carbs roughly equals one serving, and understanding this relationship helps predict how foods will affect your blood sugar. Focus on complex carbohydrates like quinoa, sweet potatoes, and oats rather than simple sugars that cause rapid spikes.
The plate method simplifies meal planning without complicated calculations. Fill half your plate with non-starchy vegetables like broccoli, spinach, or peppers. Reserve one quarter for lean protein such as chicken, fish, or tofu. The remaining quarter holds your carbohydrate choice – brown rice, whole grain bread, or beans.
Timing matters as much as food choices. Eating smaller, more frequent meals prevents dramatic blood sugar swings. Space meals 4-6 hours apart and include a small snack if needed between meals. Avoid skipping meals, which can lead to dangerous lows followed by rebound highs when you finally eat.
| Food Category | Best Choices | Portion Guidelines |
|---|---|---|
| Proteins | Fish, lean meats, eggs, tofu | 3-4 oz per meal |
| Vegetables | Leafy greens, broccoli, peppers | Unlimited non-starchy |
| Carbs | Whole grains, legumes, fruits | 1-2 servings per meal |
| Fats | Olive oil, nuts, avocado | 1-2 tablespoons |
Stay hydrated with water instead of sugary drinks. Even diet sodas can sometimes trigger cravings for sweet foods. If you drink alcohol, do so with food to prevent low blood sugar episodes.
Exercise routines designed for diabetic health
Regular physical activity acts like medicine for diabetes, often lowering blood sugar for hours after you finish exercising. Start with 150 minutes of moderate activity weekly, broken into manageable chunks. A 30-minute walk five days a week meets this goal perfectly.
Aerobic exercise burns glucose immediately and improves insulin sensitivity. Walking remains the most accessible option – no gym membership required. Swimming provides excellent full-body exercise while being gentle on joints. Cycling, dancing, or playing tennis all count as effective cardio options.
Strength training builds muscle mass that continues burning glucose even at rest. Resistance bands, free weights, or bodyweight exercises like push-ups and squats all work well. Aim for two sessions weekly, targeting all major muscle groups. Don’t worry about becoming a bodybuilder – even light weights provide significant benefits.
Pre-exercise checklist:
- Check blood sugar levels
- Have a snack if glucose is below 100 mg/dL
- Carry glucose tablets or juice
- Wear proper footwear to prevent injuries
- Stay hydrated throughout your workout
Monitor your response to different activities. Some people experience blood sugar drops during exercise, while others see increases. High-intensity workouts sometimes cause temporary spikes due to stress hormones. Keep glucose tablets handy and never exercise alone if you’re prone to severe low blood sugar episodes.
Medication options and when they become necessary
Type 1 diabetes requires insulin from diagnosis since the pancreas produces little to none. Multiple daily injections or insulin pumps deliver this life-saving hormone. Rapid-acting insulin covers meals, while long-acting forms provide steady background coverage throughout the day.
Type 2 diabetes medications work through different mechanisms. Metformin reduces glucose production by the liver and remains the first-line treatment for most people. It rarely causes low blood sugar and may even support modest weight loss. Side effects like stomach upset usually improve over time.
When metformin alone isn’t enough, additional medications join the treatment plan. SGLT-2 inhibitors help kidneys remove excess glucose through urine. GLP-1 receptor agonists slow digestion and reduce appetite. Some of these newer medications offer cardiovascular and kidney protection beyond blood sugar control.
Common medication progression:
- Lifestyle changes (diet and exercise)
- Metformin as first medication
- Add second oral medication if needed
- Consider insulin if targets aren’t met
- Combination therapy for optimal control
Don’t view medication as failure – diabetes is a progressive condition where the pancreas gradually produces less insulin over time. Starting medications early often prevents complications and maintains better long-term health. Work closely with your healthcare team to find the combination that works best for your lifestyle, budget, and health goals.
Regular medication reviews ensure your treatment plan evolves with your changing needs. Weight loss, increased activity, or other health conditions might allow for medication adjustments or reductions over time.

Diabetes affects millions of people worldwide, but understanding its causes and symptoms can help you stay ahead of potential health issues. From genetic factors to lifestyle choices, the root causes vary between different types of diabetes, making it important to recognize the early warning signs like frequent urination, excessive thirst, and unexplained fatigue. Whether you’re dealing with Type 1, Type 2, or gestational diabetes, each requires a unique approach to management.
Taking control of diabetes doesn’t have to feel overwhelming. Simple changes like monitoring blood sugar levels, maintaining a balanced diet, staying active, and working closely with your healthcare team can make a significant difference in your quality of life. If you notice any symptoms or have risk factors for diabetes, don’t wait to speak with your doctor. Early detection and proper management are your best tools for living a healthy, fulfilling life with diabetes.












